What Are Urinary Strictures?
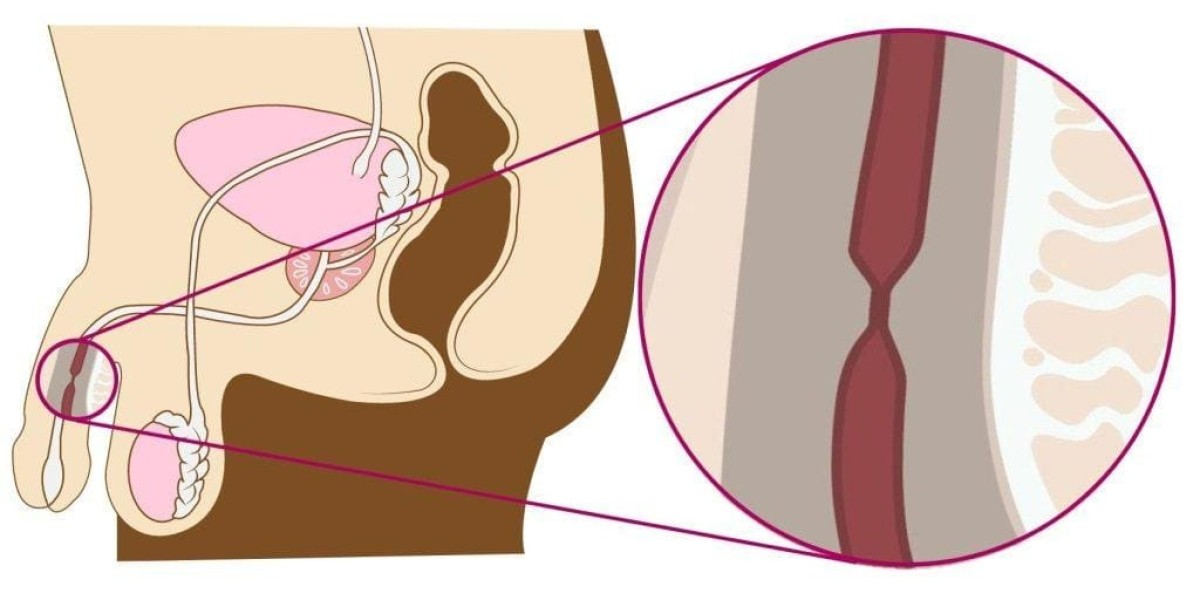
Urinary Strictures, also known as urethral strictures, occur when the urethra — the tube that carries urine out of the body — becomes narrowed or blocked. This narrowing restricts the normal flow of urine, leading to difficulty urinating, pain, and potential urinary tract complications.
The condition is more common in men than in women, primarily due to anatomical differences in the urethra. If left untreated, urinary strictures can cause repeated infections, bladder damage, or even kidney problems. Therefore, early diagnosis and treatment are essential for maintaining long-term urinary health.
Common Causes of Urinary Strictures
Several factors can lead to the development of urinary strictures, including:
Injury or Trauma:
Damage to the urethra from accidents, falls, or prolonged catheter use can cause scarring that narrows the passage.Infections:
Chronic or untreated urinary tract infections (UTIs) or sexually transmitted infections (STIs), such as gonorrhea, may lead to urethral inflammation and scarring.Previous Surgery or Instrumentation:
Medical procedures involving the urethra or prostate can sometimes cause irritation and scarring over time.Inflammatory Conditions:
Certain inflammatory diseases of the urethra can cause long-term narrowing.Congenital Defects:
Some individuals are born with a naturally narrow urethra, which may worsen with age.
Regardless of the cause, urinary strictures should always be evaluated by a urology specialist to determine the most effective treatment approach.
Symptoms of Urinary Strictures
The symptoms of urinary strictures often vary depending on the degree of narrowing. Common signs include:
Weak or reduced urine stream
Difficulty starting urination
Pain or burning during urination
Incomplete bladder emptying
Urinary retention (inability to urinate)
Frequent urinary tract infections
Blood in the urine (hematuria)
If these symptoms persist, it’s important to seek medical care promptly to avoid further urinary complications.
Diagnosing Urinary Strictures
Diagnosis involves a combination of medical history, physical exams, and advanced imaging tests to identify the location and severity of the stricture. Common diagnostic methods include:
Uroflowmetry: Measures urine flow rate to detect obstruction.
Retrograde Urethrogram (RUG): An X-ray test that uses contrast dye to visualize the urethra.
Cystoscopy: A thin, flexible scope inserted through the urethra to view narrowing or blockage directly.
Ultrasound or MRI: Helps evaluate the bladder and surrounding structures.
Treatment Options for Urinary Strictures
The treatment for urinary strictures depends on their length, location, and cause. Urologists may recommend one or more of the following options:
1. Urethral Dilation
A non-surgical procedure that involves gradually stretching the urethra using specialized instruments. It provides temporary relief but may not prevent recurrence.
2. Internal Urethrotomy
This minimally invasive technique involves cutting through the stricture using a small endoscopic tool. It’s suitable for short, less complex strictures.
3. Urethral Reconstruction (Urethroplasty)
For longer or recurrent strictures, urethroplasty is the most effective and permanent solution. This surgical procedure removes the scarred segment and reconstructs the urethra using healthy tissue.
4. Catheterization
In severe cases, temporary catheter placement helps drain the bladder and relieve urinary retention until definitive treatment is performed.
5. Follow-Up and Maintenance
After treatment, patients may need periodic monitoring to ensure the urethra remains open and urine flows normally.
Living with Urinary Strictures
Living with urinary strictures can be frustrating, especially when symptoms recur. However, lifestyle changes and regular follow-ups can make management easier:
Stay well hydrated to prevent urinary infections.
Avoid holding urine for long periods.
Maintain proper hygiene and safe sexual practices.
Follow medical advice on catheter or stent care (if applicable).
Attend regular check-ups with your urologist to monitor recovery.
Early intervention and ongoing care significantly reduce the risk of complications like bladder damage or kidney failure.
Why Early Treatment Matters
Delaying treatment for urinary strictures can lead to serious urinary and kidney issues. Prolonged obstruction may cause the bladder to weaken, making it difficult to urinate even after the stricture is treated. In advanced cases, infections can spread to the kidneys, posing a significant health risk.
Advances in urologic surgery, particularly urethroplasty, have made it possible to correct strictures with excellent long-term success rates and minimal recurrence. The earlier the diagnosis, the simpler and more effective the treatment tends to be.
Conclusion
Urinary Strictures are a common yet treatable condition that can significantly affect a person’s quality of life if not managed promptly. Modern urological care offers several effective solutions — from minimally invasive dilation to advanced urethral reconstruction — ensuring that patients can regain comfort and normal urinary function.
For individuals experiencing symptoms like weak urine flow, pain, or frequent infections, it’s essential to seek professional help. Urology Partners of North Texas provides expert evaluation and state-of-the-art treatments, including advanced urethroplasty procedures, tailored to each patient’s condition. Their skilled team is dedicated to helping men restore urinary health and find lasting relief through personalized, compassionate care.
Frequently Asked Questions (FAQs)
1. What causes urinary strictures?
They are often caused by infections, injuries, or scarring from previous surgeries. In some cases, they may be congenital or linked to long-term catheter use.
2. What are the main symptoms of a urinary stricture?
Common symptoms include a weak urine stream, pain during urination, urinary retention, and recurrent urinary tract infections.
3. How is a urinary stricture diagnosed?
Tests such as cystoscopy, urethrogram, or uroflowmetry are used to identify the location and severity of the narrowing.
4. Is surgery always necessary for urinary strictures?
Not always. Some mild cases respond to dilation or minimally invasive treatments, but recurrent or long strictures usually require surgery like urethroplasty.
5. Can urinary strictures return after treatment?
Yes, strictures can recur, especially if the underlying cause persists. Regular follow-up with a urologist helps detect and manage recurrences early.